What is adherence?
Adherence means sticking to something. It is often used to describe taking medicine without missing doses for as long as needed. Good adherence helps to maintain—or improve—your health.
This fact sheet is about adherence to hepatitis C treatment. It may be helpful for other medications, whether you are taking them for a short time, or for the rest of your life.
With hepatitis C treatment, the most important thing a person can do to be cured is not to miss taking any of their medication—and to finish all of it.
Knowing how hepatitis C treatment works—instead of just being told to take all of your medication—makes it easier to understand why adherence matters so much.
How does hepatitis C virus (HCV) treatment work?
Just like people, viruses do not live forever; they are constantly reproducing. Hepatitis C drugs work by blocking different steps in the virus life cycle; this prevents HCV from making more of itself. Once the virus stops reproducing, it dies off. After both of these things happen, a person is cured.
People need to stay on HCV treatment for a certain amount of time to make sure that drugs can get the job done. Hepatitis C treatment lasts from eight to 24 weeks. (Researchers are looking at even shorter treatment.)
 Why is adherence important?
Why is adherence important?
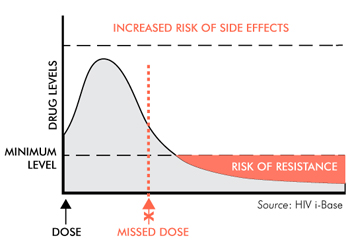
For drugs to work, there have to be enough of them in a person’s body. If drug levels get too low, the drugs won’t work; if they get too high, side effects can be worse.
What is drug resistance?
Each day, HCV makes billions of copies of itself. Some of these copies are not the same as the original virus. They have changes, called mutations. Some mutations are harmless, but others can stop hepatitis C drugs from working (called drug resistance).
When people miss doses of their hepatitis C treatment, the virus gets a chance to reproduce. Some of the copies it makes might have mutations that cause drug resistance. Drugs can stop working if changes in the hepatitis C virus make it resistant to the drugs.
Some people have drug resistance even though they have never been on hepatitis C treatment. Many of them have been cured anyway. But most people who are not cured will have resistance to one or more of the hepatitis C drugs they took. Resistance to certain hepatitis C drugs can disappear within months. But resistance to other drugs can last for years and might prevent re-treatment from working.
Why does dosing matter?
Some drugs linger in a person’s body for weeks, while others pass through it in a few hours. Researchers can see how long drugs stay in a person’s body and whether food changes this. They use this information to figure out how often drugs need to be taken. Some drugs need to be taken on an empty stomach. Other drugs need to be taken with food to work. It’s a good idea to ask whether this means with a snack or a full meal.
Some HCV drugs need to be taken only once a day. It is important to take them around the same time each day to keep enough of the drug in your system. For HCV drugs that need to be taken twice a day, it is best to take them every 12 hours—or as close to it as possible.
Drug interactions:
Some medications should not be used together. Combining them can change drug levels (called drug-drug interactions). Higher drug levels can worsen side effects. When drug levels are too low, drugs cannot do their job. Low drug levels put people at risk for drug resistance or not being cured.
Before you start hepatitis C treatment, talk with your health care provider about starting, using, or stopping any medications, supplements, or herbal remedies to avoid drug-drug interactions.
How is adherence measured?
In clinical trials, adherence is checked often, usually in more than one way. Methods used in research include:
- taking a blood sample to check medication levels;
- keeping a written record of when medication is taken;
- bringing pill bottles or blister packs to clinic visits for pill counts;
- using pill bottles with caps that track each time bottles were opened (called MEMS);
- using blister packs that track each time a pill is removed—this information can be sent to a smart phone;
- using new pill bottles that light up, buzz, and send text and voice mail messages. These can also track how many times a pill bottle has been opened and shut, and how many pills are left; and
- using edible “smart pills” to see when medication was taken.
“Smart pills” work with a patch that is worn on a person’s torso. Each smart pill has a sensor that becomes activated after it enters the stomach. When the smart pill is activated, it sends a wireless signal to the patch. Then the patch sends information (including when the pill was taken, heart rate, and how active you are) to a mobile app. The smart pills come in regular packaging or in blister packs. Depending on the pharmacy and type of medication a person uses, it may be possible to combine a smart pill with a person’s regular medication. In the future, the technology that goes with smart pills will change.
There are other, less complicated ways to support adherence. Some people leave their medication in a familiar spot (such as the bathroom or by the coffee pot). Others use pillboxes to make sure that they are taking medication at the right time. People also use alarms on their smart phones or mobile applications to support adherence.
What makes adherence difficult?
Adherence can be difficult for many reasons. Often people simply forget to take medication or refill their prescriptions. Sometimes people have other reasons for missing their medication, including:
- having side effects from medication—especially if you don’t feel sick;
- feeling better, even though you haven’t finished treatment;
- not wanting to think about why you need to take medication;
- being tired of taking medication every day;
- not wanting other people to know why you are taking medication;
- having to take several different medications, at different times, with or without food;
- loss of or change in employment and insurance;
- difficulty getting prescriptions refilled or delivered;
- money problems;
- responsibilities, including work and childcare;
- being arrested;
- having a busy or chaotic life;
- moving;
- traveling, especially when time zones are different;
- becoming homeless; and
- untreated mental illness.
It’s important not to be too hard on yourself if you forget a dose of your medication—nobody is perfect! Sometimes talking to another person who is going through a similar experience, a health care provider, or a pharmacist can help you with adherence tips and support.

