Claiming and strategizing the HIV community’s role in universal health care advocacy
By Suraj Madoori and Maximillian Boykin
 Perhaps the most impressive narrative in the lead-up to the dramatic defeats of the disastrous Affordable Care Act (ACA) repeal-and-replace bills in the House and Senate involved the thousands of activists who were activated, organized, and mobilized in an effort save U.S. health care. For months, hundreds of email alerts were sent, a deluge of phone calls made to Congressional offices, and busloads of HIV, disability, and health justice advocates bravely sacrificed their bodies on Capitol Hill in civil disobedience and direct actions, demanding that their elected officials protect their care before the ultimately doomed votes.
Perhaps the most impressive narrative in the lead-up to the dramatic defeats of the disastrous Affordable Care Act (ACA) repeal-and-replace bills in the House and Senate involved the thousands of activists who were activated, organized, and mobilized in an effort save U.S. health care. For months, hundreds of email alerts were sent, a deluge of phone calls made to Congressional offices, and busloads of HIV, disability, and health justice advocates bravely sacrificed their bodies on Capitol Hill in civil disobedience and direct actions, demanding that their elected officials protect their care before the ultimately doomed votes.
The community mobilization and advocacy to stop the legislation is a clear example of how vital the ACA has been to transforming the health and lives of people living with, and vulnerable to, HIV. However, in celebrating the defeat of these bills, we have failed as a community to further galvanize this energy to clearly project and envision the health care system that we truly need. Now is the time for us to engage in ongoing national conversations on a single-payer system that can potentially shift our current health care paradigm to one that is radically transformative, universal, cost-saving, and just for all people living with HIV (PLWHIV) and vulnerable communities.
The gains ushered in with the ACA cannot go understated, especially for PLWHIV. According to the Kaiser Family Foundation, several provisions, including removal of pre-existing conditions, elimination of benefit limits, and providing subsidies for the purchase of marketplace plans, have had direct benefits for PLWHIV and vulnerable communities in the U.S. Furthermore, the ACA works remarkably well in tandem with the Ryan White CARE Act, which acts as a critical safety net for those who fall within the ACA’s coverage gap or lose insurance.
But even with these and other important gains, there are stark challenges and uncertainties that call into question whether the ACA is the health care panacea for our communities. More than 20 million U.S. residents remain uninsured, including a disproportionate number of Black and Brown people. Undocumented immigrants are walled off. Since 2015, we have seen a reduction in the number of in ACA marketplace plans being offered through insurers, often in response to undermining and destabilizing forces. These include relentless conservative rhetoric and legislative efforts to toss the ACA, including the vital individual mandate. Then there are the executive orders ending cost-sharing reduction subsidies and the endorsement of weak subprime insurance policies.
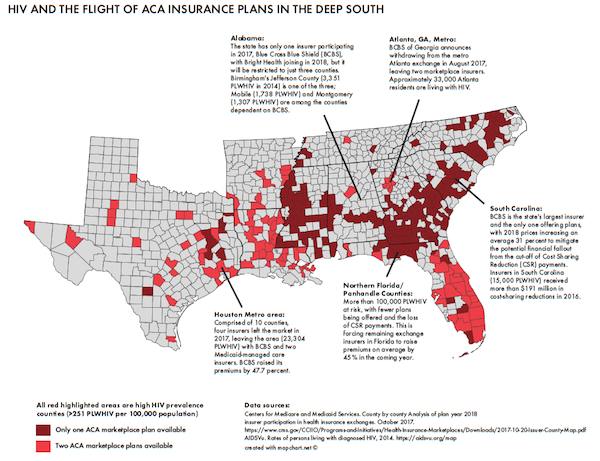
On the very heels of the American Health Care Act and the Better Care Reconciliation Act in the House, Blue Cross Blue Shield of Georgia announced on August 7 that it had withdrawn from Metro-Atlanta’s Obamacare exchange, along with 72 other counties. The move is significant, as it is yet another insurer exiting a highly vulnerable jurisdiction that is affected by HIV. These trends are being seen across HIV-affected areas in the South, with larger insurers continuing to pull back in key areas (see Figure).
The situation is made worse by many southern states not expanding Medicaid. With scarce options, many people vulnerable to HIV and other health disparities, especially young people of color, will choose to go without insurance they cannot afford—essentially negating the reason for the ACA. The retraction of marketplace plans puts the HIV community in a lurch. What good are the key ACA provisions of protecting those with pre-existing conditions, essential health benefits, out-of-pocket cost caps, and premium tax subsidies if insurance options are being depleted in highly affected areas?
The Obamacare ‘death spiral’ has certainly provided fuel for efforts to supplant the ACA, but it also provides ideal cover to shift public attention from where the ACA and health care system is most stable: Medicaid. While the insurance markets continue to bend and collapse under destabilizing forces, government-funded Medicaid stands pat.
The Center for Budget and Policy Priorities (CBPP) strengthened the defense of Medicaid against GOP proposals to restructure, cap, and block-grant the program. Research published by CBPP in June 2017 illustrates Medicaid as “efficient and effective,” particularly with improved health outcomes and increased access to health care across expansion states such as Arkansas and Kentucky. Medicaid continues to buck the trend where market-driven solutions fail, providing robust coverage and critical access to health care for numerous low-income and vulnerable populations.
Medicaid’s backbone of success, especially across expansion states, is strong federal government involvement and funding. Contrary to conservative arguments, government intervention in health care provides remarkable stability to the overall health care system while expanding access to critical health and preventive care to vulnerable communities. Supporting this notion is not only the tremendous public outcry to GOP efforts to cull Medicaid, but public polling showing that support for any government-funded health care, such as single-payer or Medicaid, is peaking. According to a June 2017 Pew Research survey of U.S. adults, 60% of respondents said the federal government is responsible for ensuring health care coverage for all Americans. A growing 33% support government-funded single-payer insurance or a mix of private and government programs. Nearly 57% of Republicans in that same poll say the government “should continue Medicaid and Medicare for the elderly or very poor,” even if they do not support increased government responsibility for ensuring health care.
Riding the wave for increased public support of government-funded health care is a slew of state and federal legislation for a public option or single-payer insurance. Much of the momentum is owed to Senator Bernie Sanders (VT), who pitched Medicare-for-All as a key plank in his 2016 Presidential campaign and recently introduced a bill in Congress, which received significant attention in this latest health care battle waged on the Medicaid and the ACA.
California is being watched closely as a state pushing single payer. Although legislation (SB-562) introduced in the State Assembly in June 2017 was ultimately put on hold, it has maintained critical support and organization coming from multiple community stakeholders. A state the size of California gaining a single-payer system may yield tremendous power to consolidate prescription drug purchasing and negotiate prices with pharmaceutical companies, a driver of rising health care costs that continues to go unaddressed by current health care schemes (see Tim Horn’s “Universal Health Care and Prescription Drug Pricing”). There’s a saying: “As California goes, so goes the nation.”
But where is the HIV community? Despite the powerful voice and mobilizing efforts of our activists and leaders in stopping the destruction of the ACA, we have missed the boat on paralleling our organizing alongside a projection of our vision on what a truly just and equitable health care system can and should be. Even more concerning is the mixed messaging we send to communities on what we are fighting for in terms of a health care system. In a recent email call-to-action issued by NMAC on August 15, a hyperlink leads to a Google form titled, “Universal Healthcare! (NOT Tax Cuts).” In the context of the attempted raids on the ACA, this raises several critical questions. What are we as a HIV community defining as universal health care (UHC)? Do we really believe that the ACA is UHC? Have we even come together as a community to agree on what UHC truly looks like for all of us? What are our responsibilities of allyship—as a movement that has earned tremendous victories for our survival through activism and advocacy—for marginalized communities that currently lack health equity and access?
These questions remain unanswered as momentum grows for a radically different health care system in the U.S. that catches up with the rest of the industrialized world, where UHC is already recognized and guaranteed. Several developments, however, have provided a glimpse of what’s possible. Without a doubt, government-funded Medicaid expansion has been critical to expand health care to PLWHIV and vulnerable communities. A board resolution from the AIDS Foundation of Chicago, for example, details that more than 13,000 PLWHIV in Illinois are covered by Medicaid. It has become the largest single payer of HIV care in the state.
Medicaid expansion, notably cross-movement organizing for continued expansion across the South, must continue as a chief strategy. The HIV community’s reliance on Medicaid positions us as a leader to support a move towards a robust, government-funded system that ensures consistent, universal access to health care, treatment, and prevention that can help drive viral-suppression and lower HIV rates. The HIV community also has the ability to show how UHC, backed by robust government support, can benefit PLWHIV and provide cost-effective strategies against conservative-minded replacement bills that only emphasize health inequity by potentially driving HIV health disparities and are not cost-effective.
 As this issue of TAGline goes to press, Democrats are aligning themselves behind the single-payer and UHC momentum generated by the attacks on health care (see Table).
As this issue of TAGline goes to press, Democrats are aligning themselves behind the single-payer and UHC momentum generated by the attacks on health care (see Table).
In late August, Senator Brian Schatz (D-HI) previewed a proposal (now called the State Public Option Act) that allows middle- and high-income earners to buy into Medicaid through Obamacare exchanges—building on the narrative of the program as a stable source of health care. Senators Elizabeth Warren (D-MA) and Kirsten Gillibrand (D-NY) have recently come out in strong support of a single-payer or public option as well.
Members of the Congressional Black Caucus (CBC), including Senator Kamala Harris (D-CA) and Representative Robin Kelly (D-IL), stand behind a single-payer option.
In October, Senators Michael Bennet (D-CO) and Tim Kaine (D-VA) proposed Medicare X, which would allow Americans to buy a public health insurance plan.
One of the chief architects of the ACA, retired Senator and former chair of the powerful Senate Finance Committee Max Baucus (D-MT), has come out in strong favor of single payer.
Given that HIV/AIDS is a strong bipartisan issue, we are well positioned to support our allies in Congress to reach across the aisle to build even more support for realizing a vision of UHC, especially for PLWHIV. Capitalizing on data illustrating how Ryan White fills critical gaps in the ACA and the effect of Medicaid expansion on the care continuum for PLWHIV can give us evidence towards how effective a UHC system can be for PLWHIV.
Without involvement and inclusion in these current debates, we risk being left behind and without the opportunity to define and inform how any system, including single payer, can meet the critical needs of PLWHIV. As the authors of this article, we do not write to convince the larger community that single payer is the one-stop solution to our health care system. Rather, we note that these national conversations towards single-payer and other UHC models are now happening and that we are failing to make our voices heard in ensuring that any proposed health system, scheme, or concept is informed by the meaningful involvement of PLWHIV and vulnerable communities.
While the fight to defend the ACA continues, so does our fight for truly UHC. Take it from the two authors, who have lost our own health insurance at one time, lost family members to not having health insurance, case-managed HIV-positive young people struggling with homelessness and no health care, led demonstrations against large insurers as students, and organized in communities that still struggle to gain the critical access to health care. UHC in each of these instances could have positively changed the trajectories of many members of these communities and our own lives. We have fought to keep the ACA because we believed it would save lives, which it has. But let’s not rest on our laurels until we have achieved true UHC for all.
Maximillian Boykin is at the HIV Prevention Justice Alliance and the AIDS Foundation of Chicago.