Advocates scramble to stay ahead of coverage rejections, formulary concerns, and exorbitant out-of-pocket expenses facing people living with HIV
By Kenyon Farrow
#GetCovered
That’s the White House’s official hashtag and marketing campaign to spike the number of Americans enrolling into qualified health plans (QHP) through the Affordable Care Act (ACA). The deadline for individual enrollment without penalty was March 31.
But many people with HIV who tried to join the ranks of the enrolled found their third-party payments—primarily Ryan White subsidies to offset monthly premiums—rejected by insurance plans. Others discovered that their drug regimens weren’t covered, leaving them with huge out-of-pocket coinsurance expenses. In short, for many people hoping that the ACA would mean better and more affordable access to treatment, April Fools’ Day came earlier than expected. But the gaps and the discriminatory practices causing them are no laughing matter.
When the ACA was signed into law four years ago, it gave many AIDS advocates plenty of hope that more uninsured people would be able to get comprehensive health coverage. The law was structured around several core principles:
- expanding Medicaid eligibility for poor single adults (including all people with HIV meeting the other Medicaid eligibility requirements);
- creating national standards for insurance plans and the services they need to offer;
- shifting our model from fee-for-service to one based on outcomes;
- bringing more people into the insurance market to balance the risk pool (through the individual mandate); and
- removing barriers to care, such as preexisting conditions clauses that have historically been used by the insurance industry to reject patients.
Prior to ACA implementation, close to 70,000 people living with HIV were uninsured. According to Kaiser Family Foundation estimates, roughly 23,000 of those would gain coverage through state or federal QHPs, the majority of whom would also qualify for financial assistance. Approximately 47,000 would be eligible for Medicaid if all states expanded the program (only 26 states have agreed, thereby reducing the number of uninsured people living with HIV gaining coverage through Medicaid by more than 40 percent). So expanding Medicaid should help many people with HIV who are poor gain critical access to health care. Opening the private insurance market to people with HIV (especially those who live in states where their HIV status made them “uninsurable”) should, in theory, greatly expand their access to treatment and care. In practice, the outcomes of these changes have been much more mixed.
Health Insurance Coverage Options under the ACA for Uninsured Adults with HIV in Care
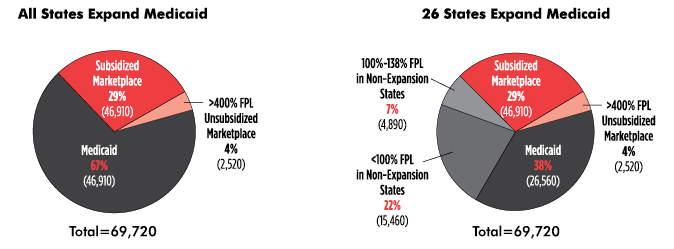
Based on state Medicaid decisions as of October 22, 2013.
Source: Kates J. Assessing the impact of the Affordable Care Act on health insurance coverage of people with HIV. Kaiser Family Foundation; 2014. Available from: http://kff.org/report-section/assessing-the-impact-of-the-affordable-care-act-on-health-insurance-coverage-of-people-with-hiv-issue-brief. (Accessed 2014 March 30)
One of the first problems to emerge was that, for many people with HIV, their HIV medications weren’t explicitly included on plan formularies or—worse, covered at all. Others found that their antiretrovirals were placed in a special tiered pricing system that offered minimal cost sharing, which translated into consumers paying as much as half of their drugs’ retail costs out of pocket as a coinsurance expense.
While many were commemorating World AIDS Day 2013, AIDS activists (including TAG) sent a letter to Health and Human Services (HHS) Secretary Kathleen Sebelius detailing the issues that were occurring, mostly (but not exclusively) with health plans in Southern states that did not establish their own state exchanges. Due to advocacy by the AIDS community, several insurers made changes to their drug formularies, but there has yet to be any movement from Secretary Sebelius on this issue.
And discriminatory practices in drug formularies with QHPs are not the only problem. Several insurance companies that have attempted to block people with HIV from signing on to their health plans. On February 25, after a class-action lawsuit was filed by Lambda Legal, a federal judge granted an emergency injunction forcing three Louisiana insurance plans to accept third-party subsidies and maintain coverage for people living with HIV, regardless of the premium payment source.
John East, a 59-year-old health care worker, had been insured by Blue Cross and Blue Shield (BCBS) of Louisiana for 30 years. He learned that his policy was being dropped because the insurer was no longer going to accept Ryan White payments. When the story first leaked, BCBS of Louisiana announced that the decision was due to ACA regulations barring them from accepting third-party payments. The Centers for Medicare and Medicaid Services rebutted the statement by saying there was no such federal policy preventing insurers from accepting payments from Ryan White.
To bolster support for federal direction on this problem, activists sent a letter to Secretary Sebelius on March 3 asking her to urgently address the issue by making the following policy changes:
- Require that QHPs accept third-party payment of premiums from government-supported programs, including the Ryan White/AIDS Drug Assistance Program, on behalf of qualified low-income clients.
- Amend the essential health benefits rules to require coverage of specialty drugs and prohibit coinsurance from exceeding 25 percent for these treatments, particularly those widely accepted as standard-of-care and for which no generic equivalents exist.
- Require all Marketplaces to ensure that QHPs provide complete and accurate formulary information in a standard format, including the actual out-of-pocket costs that will be imposed on enrollees.
But there’s some good news. On March 10, Louisiana state insurance companies agreed to continue to accept Ryan White payments through November 15, which is the end of this enrollment period. In order to ensure that people living with HIV get affordable care, however, we need policy changes that don’t rely on the benevolence of insurance companies.
On March 19, HHS published a new rule in the Federal Register entitled, “Patient Protection and Affordable Care Act; Third Party Payment of Qualified Health Plan (QHP) Premiums”; a public comment period on the rule ends in May. The hope is that the new rule will solve the issue of Ryan White premium assistance across all states. Unfortunately, the rule also encourages QHPs to reject third-party payments from drug companies, which could be a headache for Marketplace-covered people living with HIV who face high out-of-pocket costs for antiretrovirals, particular when low-cost generic versions aren’t available.
Without ensuring access to quality care that is affordable to people with HIV, we will fail in our efforts to fill the gaps in the HIV care continuum. According to the Centers for Disease Control and Prevention, 82% of all people with HIV have been diagnosed, but only 66% are linked to care, and worse, only 37% are retained in care, with 33% on antiretroviral therapy. One way to fix this is to remove policy barriers that prevent people from getting health insurance. For people who lack access to Medicaid, the continuation of Ryan White funds will be essential to efforts to get and keep people in care.
HHS must continue to actively enforce the ACA’s promise to prohibit discrimination on the basis of preexisting conditions in the insurance market. Otherwise the Obama administration’s public charge to #GetCovered will leave people with HIV out in the rain.•
