We won’t end HIV as an epidemic with anemic goals, delayed surveillance data, feeble support of state policies and resource needs, and an inadequate implementation science agenda
By Kenyon Farrow
The U.S. National HIV/AIDS Strategy (NHAS) ends its five-year run at the end of 2015 with mixed results. Due to long gaps in HIV surveillance reporting, unambitious targets, and a lack of funding, authority, and incentives to enforce the strategy—not to mention the high turnover rate of leadership at the White House Office of National AIDS Policy (ONAP) since the strategy’s inception (there have been three ONAP directors during the Obama presidency)—the impact of the NHAS itself is still unclear.
The new director of ONAP, Douglas Brooks, has announced that he’s working on an update of the NHAS to be released this year, before his tenure likely ends with the inauguration of a new president in January 2017.
At this point, any National HIV/AIDS Strategy has to help mobilize the country and lead a national discussion about what it actually means to end the epidemic domestically and what the consequences are if we fail to. In addition to providing the kinds of messaging to the larger U.S. public about how we can reduce new infections below epidemic levels, it must also develop new goals and the kind of coordination of policy within the federal agencies charged with different pieces of the strategy.
If we’re going to end the domestic epidemic, the NHAS must greatly increase and standardize targets and ensure that policies to achieve those targets are implemented at the federal and local levels. Notable examples are the low—and divergent—viral-load suppression targets. The NHAS has established HIV serostatus knowledge, linkage-to-care, and continuous engagement-in-care targets of 90%, 85%, and 80% for 2015, respectively, for all major race/ethnic and risk factor groups. Yet the viral-load suppression goal is below 50%: 39.2% of blacks/African Americans, 43.9% of people who inject drugs, and 48.8% of men who have sex with men. Not only are these targets unambitious, particularly when they are expressed as percentages of people living with HIV who know their status and have been linked to care, but they buttress the health disparities that have long plagued populations most heavily affected by HIV.
Another significant limitation of the NHAS, particularly with respect to measuring its impact, is the glacial pace at which annual surveillance data are reported to the Centers for Disease Control and Prevention by state health departments and, ultimately, made available to the public by the federal agency. In recent years, reporting of most NHAS indicators has been on a three-year lag—too slow for any kind of relevant program planning, targeted funding adjustments, or prompt response to emerging epidemics. There have been many changes in our society in the last three years that affect the HIV epidemic (e.g., the rollout of the Affordable Care Act; expanded access to and education about pre-exposure prophylaxis; even the rapid emergence of social media and phone hook-up apps that may influence sexual behavior). Relying on old data will not help us rapidly evaluate, and respond to, these major shifts in HIV care and prevention service delivery, or appropriately change the course of programs or targeted resources.
Luckily, this is one area where the CDC is expected to make progress. Eugene McCray, director of the Division of HIV/AIDS Prevention at the CDC, has announced that beginning this year, annual surveillance reports will be available within one calendar year of the time that data are collected. To streamline this process, however, states must scale up their capacity to provide these data to the CDC in a timely fashion. Annual incidence estimates, however, will still go through a peer-review process and will be on approximately an 18-month lag (the peer-review process adding about six months to the publishing cycle).
Though ONAP and the CDC released interim reports on the NHAS in late 2013, hailing successes on most indicators, the bulk of their evidence drew from data that preceded the implementation, or occurred during the first six months, of the strategy. Falling incidence and improved clinical outcomes for some populations nationally can be attributed to the efforts of many states long before the NHAS was implemented. The expansion of Medicaid and other health coverage to larger portions of the population in places like Massachusetts, San Francisco, and New York, as well as strategies to accelerate access to care for people newly diagnosed in Washington, D.C., and other areas, all contribute to reductions in incidence.In addition, new research has shown that patients in many Ryan White clinics across the country are experiencing better clinical outcomes across the continuum than those receiving care in other settings.
Now, with New York, Washington State, and San Francisco advancing ambitious plans to end the epidemic in those jurisdictions, the NHAS could be critical to leveraging federal resources to implement regional as well as national plans. Additionally, there could be mechanisms in place to encourage states to develop and implement plans. One huge problem, of course, is that Medicaid expansion, as initially envisioned in the Affordable Care Act, is a critical component of reducing HIV incidence and expanding access to treatment for people with HIV. Though this decision is out of the hands of the federal government, a revitalized NHAS could provide a framework for the kinds of state policies needed to end their epidemics.
THINKING BIG: Reducing New HIV Infections
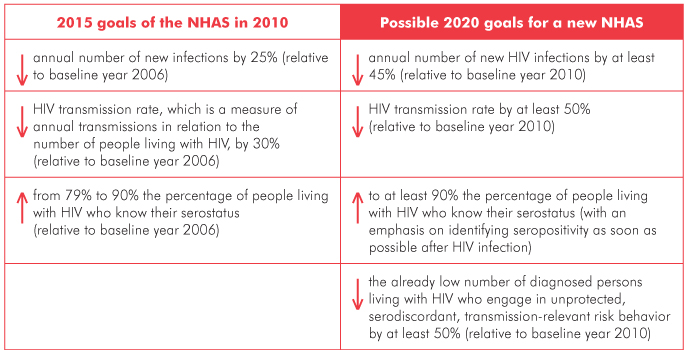
Where there is agreement among stakeholders that the original 2015 goals are conservative—and likely unachievable, given that appropriate funds were not invested in key programmatic areas—there is not yet consensus regarding the targets that might be realistically achievable, with sufficient investment, in a revitalized NHAS. To foster this discussion, David Holtgrave of the Johns Hopkins Bloomberg School of Public Health has proposed an updated NHAS for 2020, based on mathematical modeling yielding goals that are bold yet achievable. Presented here are goals pertaining to HIV incidence, with the original 2015 goals listed on the left and Holtgrave’s proposed targets on the right.
Source: Holtgrave DR. Development of year 2020 goals for the National HIV/AIDS Strategy for the United States. AIDS Behav. 2014 Apr;18(4):638–43. doi: 10.1007/s10461-013-0579-9.
We have effective interventions for quickly diagnosing HIV, improving engagement in care, and safely and effectively treating people living with HIV. What we don’t yet know is how to efficiently and effectively scale them up in all heavily affected areas and populations. It is here that implementation science—operational and dissemination research; cost-effectiveness, modeling, and economic evaluations; research to strengthen personnel and health systems; comparative effectiveness, evaluations of the impact of policy changes on public health outcomes; etc.—is not only useful, but critical. For instance, how much would diagnosing more acute infections with fourth-generation HIV tests at health departments and in clinical settings increase our rate of people who are diagnosed? What impact would that have along the care continuum?
These are some of the questions that implementation research can help us address—in ways that could help us target resources that would better meet the goals of the strategy. The Office of AIDS Research is putting into action a research agenda that includes implementation science, and we must ensure that the findings are used to effectively scale up federal, state, and local policies, programs, and funding streams.
The new NHAS will also have to more explicitly identify populations and jurisdictions that need resources and support to address their epidemics and what the federal government should do to support affected communities. That means scaling up strategies to curb transmission among black gay and bisexual men, transgender women of color, and other groups for whom traditional efforts have failed.
NHAS should be more than a skeletal framework of limp ambitions. It should be a mechanism for accountability at all levels, with an eye toward ending the epidemic. Not simply controlling it.•
