Maintaining and expanding the accomplishments of the past depend on a fight for their survival and growth—now more than ever
By Mark Harrington
 Today’s political situation with respect to the struggle to end HIV/AIDS, to treat all of those infected, and to reduce new transmission of the virus to zero, is facing new and unprecedented challenges. In this situation—particularly in the United States, where over 1.2 million people are living with HIV, where approximately 40,000 people are newly infected each year, and where over 6,720 people died of AIDS in 2014—HIV care, treatment, prevention, and support programs are likely to come under unprecedented threat from adverse political forces that are now overwhelmingly predominant in all of the branches of the federal government and in at least 33 states, which are marked by single-party dominance of the governors’ and legislative houses.
Today’s political situation with respect to the struggle to end HIV/AIDS, to treat all of those infected, and to reduce new transmission of the virus to zero, is facing new and unprecedented challenges. In this situation—particularly in the United States, where over 1.2 million people are living with HIV, where approximately 40,000 people are newly infected each year, and where over 6,720 people died of AIDS in 2014—HIV care, treatment, prevention, and support programs are likely to come under unprecedented threat from adverse political forces that are now overwhelmingly predominant in all of the branches of the federal government and in at least 33 states, which are marked by single-party dominance of the governors’ and legislative houses.
The HIV community is facing a political emergency unparalleled since the epidemic’s earliest years, in the early 1980s, when there was no prevention, little research, no effective treatment, no government funding, no public supportive services, few or no legal rights and protections, and massive fear, stigma, and discrimination, and ongoing violations of human rights of people with HIV and those at risk for HIV.
Looking more broadly on the potential effect of the new Presidency and Congressional majorities on health, a recent article in The Lancet asked “What will [the current] presidency mean for health? A scorecard.”
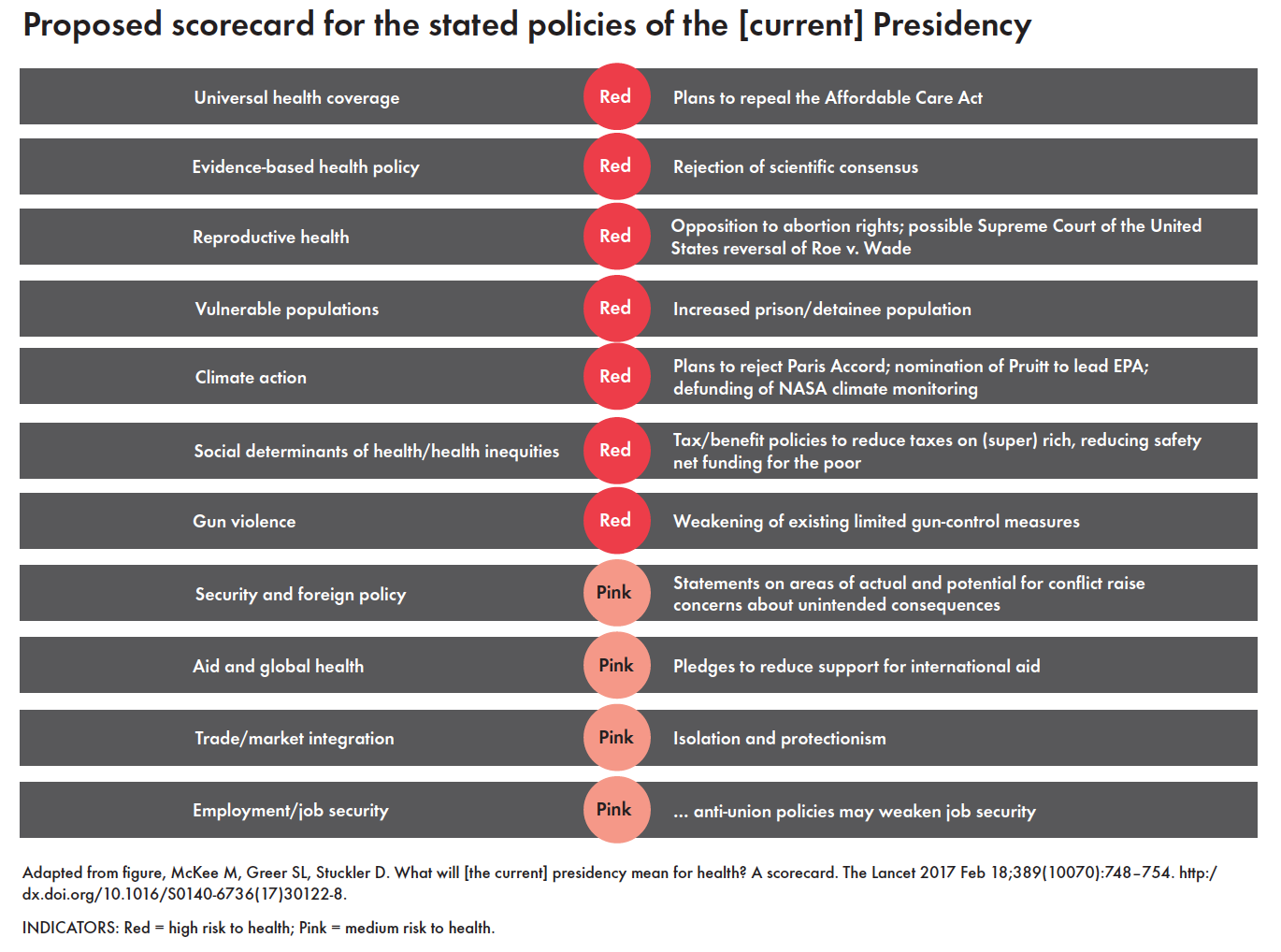
Click for larger version of table
However, our current knowledge and the scientific discoveries of the past 35 years amount to a revolutionary improvement from the unstudied state of the HIV pandemic in the 1980s: the enormous progress that has been made in understanding the science of HIV, how it is transmitted, and how it may be prevented, how it can be treated, as well as ongoing research efforts to define better prevention, treatment, a cure, and a vaccine.
There is as well an extensive, nationwide and global network of expert practitioners and providers, educated and empowered communities, and strong and diverse funding streams that support both domestic HIV treatment and care, such as the Ryan White CARE Act and the Housing Opportunities for Persons with AIDS (HOPWA) program; and global programs, such as the Global Fund to Fight AIDS, Tuberculosis, and Malaria and the President’s Emergency Plan for AIDS Relief (PEPFAR). There are large and well-organized research programs such as those administered by the National Institutes of Health (NIH) and many other research agencies.
As a result of the billions of dollars invested in research, political mobilization, and institutional growth and development that have accompanied the advent of effective prevention and treatment for HIV, death rates from AIDS have dropped almost 90 percent in the U.S. from the early 1990s (>50,000 per /year) to 2014 (6,720/year), with new infections dropping from >140,000 (1984) to <40,000 (2014). While major work remains necessary to bridge the diagnosis/treatment gap, treat everyone earlier, and scale up pre-exposure prophylaxis (PrEP) and other prevention methodologies, the US could be on a trajectory to end AIDS an as an epidemic by 2025 if the most ambitious programs—such as those in New York, San Francisco, and Washington, D.C.—are expanded and emulated.
Globally, more than 18.5 million people—or about 50% of those in need—currently receive life-saving anti-HIV treatment. As reported by Jon Cohen in the December 9, 2016 issue of Science, recent data from high-burden southern African countries such as Malawi, Zambia, and Zimbabwe indicate that treatment success (measured as virologic suppression) in PEPFAR-supported programs exceeds 85 percent—comparable to the most favorable levels in developed countries.
All of these gains are fragile. In spite of Congress’ inability to repeal the Affordable Care Act (ACA), continuing efforts to undermine domestic health programs—particularly those serving marginalized populations including people with or at risk for HIV—have the potential to severely damage HIV prevention and treatment programs. Current levels of support for Ryan White AIDS Drug Assistance Programs are vulnerable. Rewriting regulations to weaken Medicaid or to impose employment requirements where, in many places, jobs are unattainable, could hurt people with HIV and other vulnerable populations. Cuts to the U.S. Centers for Disease Control and Prevention (CDC) and NIH will damage HIV research as well as research on emerging pathogens, while cuts to the U.S. Food and Drug Administration would weaken rigorous regulatory oversight of product development. Cuts to PEPFAR and the Global Fund could throw millions off of HIV treatment, with corresponding increases in progression to AIDS, death, and new infections.
The most relevant history lesson from the 1980s, however, is that community mobilization and activism are essential for mobilizing national and state leadership, funding, resources, and political will to respond to the pandemic, protect the uninfected, treat those living with HIV, and invest in the domestic and global research, prevention, and treatment programs that ultimately have the potential to end the epidemic.
These are monumental historical accomplishments and we must fight for their sustained survival and growth with all our might.
All the progress we’ve made in the past 35 years of the global AIDS pandemic has been built on a strong foundation of community responses. We will need to be smart, agile, rapid-reacting, flexible, and willing to build new alliances and coalitions to defend all of the lives now at stake, and to ensure that we build on scientific progress to move HIV and AIDS closer than ever to their endgame.
