By Safiqa Khimani and Mark Harrington
Global political will to combat tuberculosis (TB)—once again the world’s leading killer infectious disease—may be increasing as shown by intensified activities leading to the upcoming United Nations (UN) High-Level Meeting (HLM) on Tuberculosis in September 2018.
The build-up to the HLM included the Global Ministerial Conference on Ending Tuberculosis in the Sustainable Development Era—held in Moscow, Russian Federation, in November 2017—which endorsed the World Health Organization’s (WHO) End TB Strategy targets, an 80 percent decrease in the number of new TB cases and a 90 percent decrease in TB deaths by 2030.[1]
To ensure the success of the TB HLM, TAG and its allies are working to ensure that the resulting UN General Assembly Political Declaration includes clear commitments to expand the quality and breadth of TB programs and to increase investment in research and development (R&D) necessary to make it possible to eliminate TB as a global health threat.
The UN General Assembly has held four previous health-focused HLMs, including the Special Sessions on AIDS (UNGASS) in 2001 and 2006. The 2001 UNGASS paved the way for the launch of the Global Fund to Fight AIDS, Tuberculosis, and Malaria, which has made considerable investments in all three disease areas and has saved more than 22 million lives as of 2016.[2]
The first-ever HLM on TB could be a pivotal moment to raise the bar for countries and donors on TB. UN member states now must come together to commit to investments required to meet the goals of the Stop TB Partnership’s Global Plan to End TB: Paradigm Shift 2016-2020.[3]
Current diagnostics and drug therapies will not be sufficient to achieve the required reductions in mortality and incidence. If the current rates continue, there will be 135.2 million new TB cases and 20.8 million deaths from TB by 2030.[4] New drugs and diagnostic tests that have been developed over the past 15 years are only a start towards meeting these goals. Research and development must therefore be a critical focus of the HLM. The declaration that emerges from the UN HLM must endorse innovative mechanisms for revitalizing efforts to increase funding to expand the pipeline and commit to implementing a comprehensive, integrated, ambitious, high-quality TB research agenda that goes beyond the 2015 Global Plan to End TB.
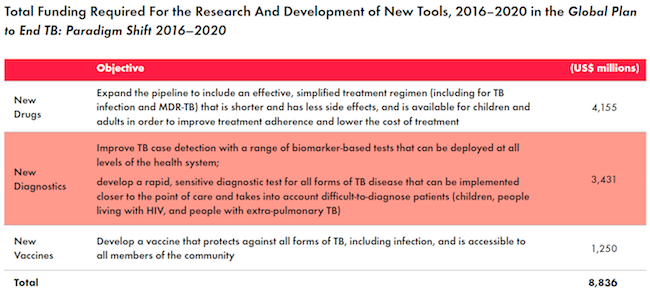
2016 global investments in TB R&D exceeded $700 million for the second time since 2005; however, this still falls short to the annual $2 billion investment needed to achieve the Global Plan’s R&D targets.[5] Thus, countries must exceed the Global Plan’s five-year funding target of $8.836 billion to increase support for basic science and operational research to catalyze progress. TAG recommends a global commitment of $10 billion to make headway on research priorities. Governments and relevant stakeholders must tap into new funding streams to meet this target.
Country-specific funding targets would allow national governments to contribute towards the $8.836 billion global goal to invest in TB R&D. This would enable them to prioritize their own country’s needs through tangible national plans while investing in the global response. A public, quantifiable commitment will make it easier for civil society to hold their governments accountable and demand that necessary actions be taken in the fight against TB.
The BRICS countries—Brazil, Russia, India, China, and South Africa—announced the establishment of a TB Research Network just before the Global Ministerial Conference; this was one of the few concrete pledges made in November. The BRICS TB Research Network aims to support and sustain collaboration, mobilize resources, and implement evidence-based TB care in these countries. This unified commitment allows BRICS countries to leverage new funding sources and go beyond the investments from the top two funders of TB R&D: the U.S. government and the Bill and Melinda Gates Foundation.[6] The network has the potential to create a model that other countries could emulate.[7]
Although greatly increased funding is vital to ensuring that TB R&D needs can be met, a comprehensive, integrated, and ambitious research agenda will be essential to provide a clear and cohesive strategy amongst the TB community.[8] The research agenda must span the full continuum of the pipeline, including basic science and biomarker discovery, new diagnostic tests, drugs and treatment regimens, vaccines and preventive therapies, and implementation science to define how best to use new tools in programmatic settings.
The pace of product development in TB has been incremental rather than transformational, despite the advances in the TB pipeline, such as the urine LAM dipstick—a simple test to diagnose TB in hospitalized HIV-positive patients—and the first approval of two new drugs from novel classes to treat TB.[9,10] Lack of investment has dramatically slowed the actions needed to bend the epidemic curve towards achieving the global goals. The Global Plan strategy on R&D outlines the specific funding required to implement the key objectives and proposes specific tools that need to be developed to narrow gaps in research (see table).[11]
TB researchers have made noteworthy progress with the introduction of two new drugs into programs for drug-resistant TB. Other new approaches include the NIX-TB trial, which uses just three all-oral drugs to treat extensively drug-resistant TB (XDR-TB).[12,13] If these results are confirmed in larger studies and in programmatic practice they will mean a major breakthrough in simplifying and shortening treatment of XDR-TB.
Accelerating a medical breakthrough such as this requires new financing mechanisms to fund research on TB. We could be nearing a transformative turning point in the struggle against TB. We must intensify our efforts to ensure that the upcoming UN HLM on TB creates meaningful momentum in research and programs to end the disease.
References
- World Health Organization. The END TB Strategy. 2015. http://www.who.int/tb/End_TB_brochure.pdf?ua=1
- The Global Fund to End HIV, Tuberculosis, and Malaria. Impact [Internet]. 2017 (cited 2018 February 18). https://www.theglobalfund.org/en/impact/
- Stop TB Partnership. The Global Plan to End TB: Paradigm Shift 2016-2017. 2015. http://www.stoptb.org/assets/documents/global/plan/GlobalPlanToEndTB_TheParadigmShift_2016-2020_StopTBPartnership.pdf
- World Health Organization. Global tuberculosis report 2017. Geneva 2017. http://www.who.int/tb/publications/global_report/en/
- Frick M. The Ascent Begins: Tuberculosis Research Funding Trends. Edited by Mark Harrington and Erica Lessem. New York: Treatment Action Group; 2017.
- Lessem E. Using lessons learnt from HIV, how do you see civil society and advocacy communities’ role in helping increase financial commitment by the global community to close the gap of TB R&D funding? Presented at: the WHO Global Ministerial Conference on Ending TB. 2017 November 17; Moscow, Russia. https://www.treatmentactiongroup.org/content/remarks-erica-lessem-tb-research-who-global-ministerial-conference-ending-tb
- World Health Organization. Global Investments in Tuberculosis Research and Development: Past, Present, and Future. Geneva: World Health Organization. 2017.
- World Health Organization. The END TB Strategy. 2015. http://www.who.int/tb/End_TB_brochure.pdf?ua=1
- Ibid.
- Frick M. The Ascent Begins: Tuberculosis Research Funding Trends. Edited by Mark Harrington and Erica Lessem New York: Treatment Action Group; 2017.
- Stop TB Partnership. The Global Plan to End TB: Paradigm Shift 2016-2017. 2015. http://www.stoptb.org/assets/documents/global/plan/ GlobalPlanToEndTB_TheParadigmShift_2016-2020_StopTBPartnership.pdf
- TB Alliance. Our Pipeline: Nix-TB [Internet]. 2018 (cited 25 February 2018). https://www.tballiance.org/portfolio/trial/5089
- Low M. The Tuberculosis Treatment Pipeline: A Breakthrough Year for the Treatment of XDR-TB. In: Frick, Gaudino A, Harrington M, Horn T, et al.; Treatment Action Group. 2017 Pipeline Report. New York: Treatment Action Group; 2017. http://www.pipelinereport.org/2017/tbtx
