Using human rights to strengthen TB research and access
By Mike Frick
Editor’s note: The following is based on the transcript of a plenary address delivered by the author at TB2016, a two-day TB conference held before the July International AIDS Conference in Durban, South Africa.
The close connection between tuberculosis (TB) research and human rights is something that civil society and TB-affected communities have already recognized and articulated. It’s an idea that TB activists, led by our comrades in South Africa’s Treatment Action Campaign (TAC), have taken to the streets. At the 46th Union World Conference on Lung Health in Cape Town, South Africa, TAC organized a march of over 500 people under the rallying cry “invest in TB R&D”. The marchers called on political leaders of the BRIICS countries—Brazil, Russia, India, Indonesia, China, and South Africa—to triple their funding for TB research, delivering an urgent reminder to these politicians that their people are still dying of TB.
The close connection between human rights and TB research has also been recognized in Geneva, where one of the foundational planks of the World Health Organization (WHO)’s End TB Strategy—protecting and promoting human rights, ethics, and equity—upholds the strategy’s three pillars of interventions, including intensified research and innovation. So TB activists have voiced demands for increased investment in TB science on the basis of human rights consequences, such as loss of life, and the WHO has suggested that there is a connection between protecting and promoting human rights and TB research. But understanding the demands of TB activists and the aspirations of the WHO’s End TB Strategy requires understanding what we talk about when we invoke rights. Human rights are more than vague aspirations or ideals. They refer to specific entitlements that are timeless, fundamental to the human person, and defined by international law. As such, human rights primarily concern the relationship between individuals and their governments, which are charged with upholding rights through a set of actions we refer to as respecting, protecting, and fulfilling rights.
Discussions about human rights and TB research are often limited to the observation that the conduct of research must respect medical ethics and rights. But beyond ethical research conduct, TB research affects human rights in a number of ways. TB research, and access to its benefits, can either reinforce or resolve ethical dilemmas in TB prevention, diagnosis, treatment, and care. Consider how the slow progress in TB drug development has left people with TB reliant on poorly performing, poorly tolerated regimens that complicate adherence in ways that raise a host of ethical issues that TB programs must navigate. TB research can also change the way that TB is culturally perceived. Imagine having the power to work against fear and stigma if the message that TB is curable were widely known. Imagine the reverse: the gains against stigma and fear that could be rolled back if, due to a lack of research, what was once curable becomes more chronic and deadly, as is happening with the rise of drug-resistant TB.
Research can also galvanize advocacy and clarify legal petitions for redress of TB-related harms. We’ve seen that happen in two landmark court cases this year. In Kenya, the High Court ruled that sending people with TB to jail to ensure adherence is not consistent with human rights standards, a decision that confirmed what should be self-evident: TB is not a crime. In South Africa, miners won the right to act as a class in their litigation against gold mining companies for failing to protect them against silicosis and TB. Both cases drew heavily on the science of TB transmission. Finally, research can either reinforce or resolve inequities that drive the TB epidemic. Think about who has access to clinical trials, how research is regulated, and the difficulties of ensuring that the products of research—new tools for fighting TB—reach all of the people in need.
Human rights also hold the potential to strengthen advocacy for intensified research and innovation by setting higher standards that research activists can appeal to and by establishing the legal duties of governments in regard to science. Within international human rights law, two rights have particular relevance for advancing research. The first is the right to the highest attainable standard of health (e.g., Article 12 of the International Covenant on Economic, Social, and Cultural Rights [ICESCR]). The right to health, in part, charges governments with ensuring that the conditions conducive to a healthy life are in place, including the availability of health goods and services. Where inadequate or outdated tools hinder a vigorous public health response to an epidemic, fulfilling the right to health may require governments to ensure the availability of health technologies by promoting the research required to create them.
The second human right with the potential to advance TB research is the right of everyone to enjoy the benefits of scientific progress and its applications (e.g., ICESCR Article 15). Under this right, scientific progress does not just refer to the general knowledge that accrues from scientific discovery, but instead extends to the actual applications of knowledge. In medicine, applications of scientific progress often take the form of tangible benefits—e.g., new disease-fighting tools. In keeping with the human rights principle of non-discrimination, all people are entitled to enjoy the right, and particular attention must be paid to vulnerable and marginalized groups. ICESCR Article 15 tasks states with two obligations: to develop science and to diffuse it. In other words, development and diffusion are distinct, yet related, steps to be taken on the same plane of concern for governments.
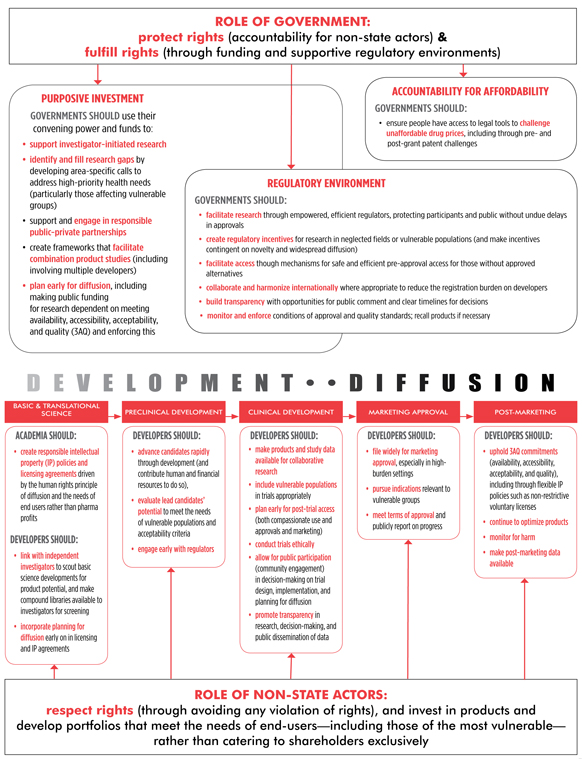
What do development and diffusion entail? According to a 2012 report by the UN Special Rapporteur in the field of cultural rights, development points to public investment in science. Diffusion refers to the dissemination of scientific knowledge and its applications, not just within the community of scientists, but within society as a whole. Human rights scholar Audrey Chapman has outlined a number of steps that governments can take to promote the development and diffusion of science and to introduce accountability mechanisms so that the public can hold state and non-state actors accountable for taking these steps.
- Set priorities for public funding and channel sufficient investment in a “purposive development of science and technology” to meet the needs of disadvantaged groups.
- Establish regulatory schemes to oversee the conduct of research and to evaluate products developed elsewhere, allowing for their importation to the benefit of constituents.
- Create opportunities for public participation in science. This starts with acknowledging that individuals have the right to participate in research as more than just clinical trial participants and that the public has a role to play in scientific agenda setting and the translation of science into policy and practice.
- Devise programs to ensure that the benefits of science are equitably distributed.
For more on the obligations of non-state actors, see “Who’s Responsible? Pharma’s Obligations Under the Right to Science” by Erica Lessem and Brian Citro.
So how are governments doing when it comes to the development and diffusion of TB science? Not very well. Global funding for TB R&D is woefully inadequate. It has never exceeded US$700 million per year globally and has remained flat since 2009, falling behind the pace of inflation. Moreover, funding is highly concentrated among a few institutions. In 2014, 50 percent of the US$674 million spent on TB R&D came from just two organizations: the U.S. National Institutes of Health and the Bill & Melinda Gates Foundation. Whether governments recognize their obligation to develop TB science is critical, as TB research depends on public budgets. Sixty percent of all money spent on TB research in 2014 came from public agencies, a reliance that has only intensified since 2011, the year when pharmaceutical companies began to pull out of TB research (combined, industry spent US$100 million on TB R&D in 2014 compared with US$145 million in 2011).
What are the consequences of limited funding for human rights? It limits the equity proposition of TB research from the outset. It also means that compromise is woven into the fabric of TB research itself. There is a real sense at TB research meetings that investigators are conditioned to think not just in terms of efficiencies, but actual scarcities. This has created an assumption of austerity that has affected how the field prioritizes different research objectives. For example, there is little money for research to meet the needs of the groups most vulnerable to TB: pregnant women, children, people who use drugs, and people with HIV. Limited funding has also affected the quantity and quality of TB science. Compare the number of studies behind the new TB drug delamanid with those behind dolutegravir, one of the newest antiretrovirals. By the time dolutegravir received approval, it had completed or initiated 61 studies, compared with six for delamanid. This disparity partly reflects differences in funding. In 2011, the world spent more than US$2 billion on HIV drug development, compared with under US$300 million on TB drug development in 2014. In terms of innovation, TB is not keeping pace with its sister epidemic, a fact borne out by U.S. Food and Drug Administration (FDA) approvals. Since 1987, the FDA has approved over 37 drugs, formulations, or drug combinations for HIV, compared with just two drugs for TB.
So that’s the development story. How are governments doing in terms of their other obligation: diffusion? Here, too, things are not looking good. A survey of 24 countries conducted by Médecins Sans Frontières revealed that national TB policies are seriously out of step with global guidelines. Of 24 countries surveyed, only 30 percent had policies to ensure that rapid molecular tests are used as the initial diagnostic for everyone evaluated for TB, only 12 percent had all of the drugs used to treat drug-resistant TB on their national essential medicines list, and only 65 percent had a process in place to access the newest TB drugs for patients out of other options. So whether it’s old technologies or new technologies, governments have failed to diffuse the benefits of TB research in policy and practice.
In an article published in the American Journal of Public Health in 1999, Paul Farmer singled out the imperative to place the right to scientific progress alongside the right to health to advance human rights and medicine. With the example of drug-resistant TB in the Russian prison system in mind, he wrote: “[what we need is] an agenda for research and action grounded in the struggle for social and economic rights, an agenda suited to public health and medicine whose central contributions for future progress in human rights will be linked to the equitable distribution of the fruits of scientific advancement.”
More than 15 years later, we have yet to firmly link science to human rights. We are still in need of an agenda for “research and action” to meet the challenges of TB and other diseases.•
