By Lindsay McKenna, Mike Frick, and Mark Harrington
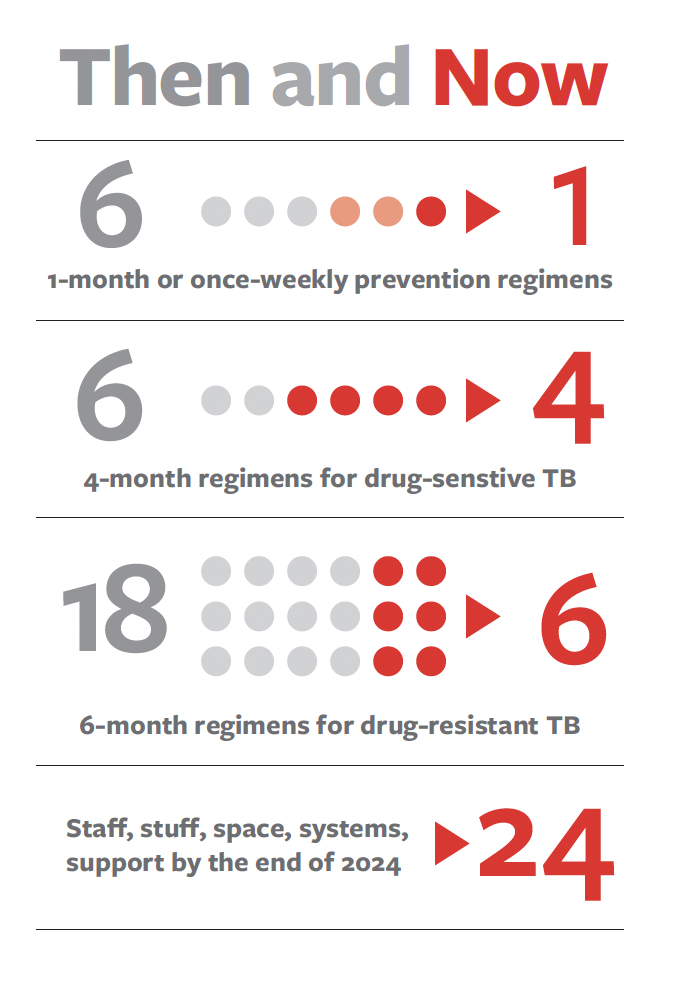
At the 24th International AIDS Conference in Montreal this summer, TAG, Partners In Health (PIH), and Médecins Sans Frontières (MSF) launched the 1/4/6×24 Campaign to accelerate equitable global uptake of newly discovered safer, shorter regimens to cure all forms of tuberculosis (TB). The “1,” “4,” and “6” represent the shortest available regimens for TB: one month or once-weekly preventive TB treatment (TPT), four months for drug-sensitive TB, and six months for drug-resistant TB. The “24” sets a deadline — the year 2024.
When TAG first added TB to its mission in 2000, global and national health actors faced strong inertia and were making little progress against the world’s oldest pandemic. Over two decades later, there has been substantial scientific advancement, and we finally have evidence-based and World Health Organization (WHO) recommended short- course regimens for the prevention and treatment of TB. And yet, far too few people who could benefit from these regimens have access to them. The 1/4/6×24 Campaign is a rallying cry to change that, in memory of Dr. Paul Farmer’s lifelong fight to extend the highest attainable standard of care and health to marginalized people across the world.
The coalition championing 1/4/6×24 urges global health actors to fulfill existing promises: In 2018, political leaders gathered during the United Nations General Assembly and committed, by 2022, to put at least 30 million people on TPT and to treat 40 million people with drug sensitive TB, including 3.5 million children, and 1.5 million people with drug-resistant TB, including 115,000 children. Four years later, and now just a few months before the end of 2022, we are not on track to meet a single target. In fact, the combined effects of the COVID-19 pandemic and other concurrent global health, economic, environmental, and political crises have reversed a generation’s worth of progress. For the first time since 2005, the number of TB deaths each year is rising. It’s against this backdrop and with an eye toward the next UN High-Level Meeting on TB in 2023 that we move forward with the 1/4/6×24 Campaign.
By rallying around the 1-month and once weekly short- course TPT regimens, the 4-month drug-sensitive TB regimens, and the 6-month drug-resistant TB regimens in a joint demand to governments and duty bearers, we aspire to reenergize the TB movement. As Dr. Farmer emphasized, ensuring universal access to scientific advances like the shorter TB regimens at the core of the 1/4/6×24 Campaign requires a few essential ingredients he dubbed “the five S’s”: staff, stuff, space, systems, and support.
“Paul used the five S’s: the first S is the space. Do you have a dignified space to receive that patient? Do you have enough staff to take care of that patient and make sure that staff have the knowledge they need? Do we have enough stuff — not only the drugs but also the diagnostics. Do we have the system? … And the last, which is the most powerful, is the social support … As Paul taught us, this campaign must deliver these regimens within a comprehensive model of care. Today we need — we must — invest in those 5 S’s.”
—Patrick Ulysse, Chief Operating Officer, PIH
With the advent of 1/4/6×24, TAG’s TB work comes full circle. In the early 2000s, TAG worked with the Treatment Action Campaign (TAC) and other allies to make the same antiretroviral medications (ARVs) for HIV that were available in the United States accessible to communities in South Africa and other low- and middle-income countries. Through this experience, TAG came to understand the deadly impact of people who, with access to ARVs, would otherwise survive HIV, as well as the dire state of TB programs and research. TAG expanded its TB work soon after in hopes that activism could change the trajectory of TB just as it had for HIV. At the time, nearly two million people were dying of TB each year, diagnostic tools dated back to the 1800s, the only available vaccine was from the 1920s, and there had not been a new drug from a new class developed for TB in over 40 years.
“There are similarities to the position we’re in now [with TB] to the [position] the world was in in the early 2000s [with HIV], when we began working with Farmer. The similarity is that we have regimens that are proven to be simpler and shorter than we’ve ever had before. They have all been proven through RCTs [randomized controlled trials] over the last 10 years to be safe, well tolerated, effective in most — but not all — people.”
—Mark Harrington, TAG
The early 2000s was also the era of “3×5” – a WHO and UNAIDS initiative that aspired to provide HIV treatment to three million people living with HIV in low- and middle-income countries by the end of 2005. Led by Jim Kim, a cofounder of Partners In Health and, for a time, the director of the WHO HIV Department, 3×5 was described by Kim as a step towards a goal of making universal access to HIV treatment and prevention accessible to all who need them as a human right. The 1/4/6×24 Campaign references more than just its predecessor’s name – like 3×5, the slogan focuses on treatment but the Campaign makes broader demands for the 5 S’s to make them possible. The 1/4/6×24 Campaign’s vision for how to change the trajectory of the TB pandemic draws inspiration from past experience doing the same for HIV. TB remains the leading infectious disease killer after COVID-19; one in four people living with HIV still die of TB. Although the tools we have to fight TB have improved dramatically over the course of the last 20 years, the political will essential to halt unnecessary suffering and preventable deaths from TB has not materialized.
The 1/4/6×24 Campaign aims to change that by using the shorter regimens as a collective priority around which the TB community can rally the energy, political will, and funding needed to end TB by 2030.
The researchers, clinicians, program representatives, and activists that spoke during the 1/4/6×24 Campaign launch in Montreal offered insight into the struggle to make today’s short-course regimens available for everyone, everywhere:
“We’re so excited to see that we can now have a six-month treatment for DR-TB, but at the same time it’s a strange feeling for me because this is a time when the excitement of achieving that scientifically in clinical trials should be dampened by the outrage that there are so many patients who need to access this and need to access it now.”
—Bern-Thomas Nyang’wa, Medical Director of MSF Operational Centre Amsterdam and Chief Investigator of TB-PRACTECAL trial.
“Rather than creating these long, laborious consultative processes. If there’s been an evidence review by WHO, then there needs to be in country a process for rapid adoption for WHO-recommended regimens. … We need targets for all those who are eligible [for 1/4/6] and those need to be incorporated in our national strategic plan.”
—Norbert Ndjeka, Chief Director of TB Control and Management, National Department of Health in South Africa and Harry Hausler, Chief Executive Officer, TB HIV Care, South Africa
“We need to call for national guidelines to reflect 1/4/6 by the end of 2022 … and for national strategic plans to reflect 1/4/6 goals. We need the Global Fund to show the way and to pay for it. … And can we find funding for national advocacy for crying out loud.”
— Sharonann Lynch, O’Neill Institute for National and Global Health Law, Georgetown University
“Today the science is on our side. This campaign could not have come at any better time than now.”
— Vuyiseka Dubula, Stellenbosch University, Africa Centre for HIV/AIDS Management, former TAC General Secretary
“We’re not going to debate about whether we’re going to do this campaign. We’re going to debate how we do it.”
— Madhukar Pai, Canada Research Chair in Epidemiology & Global Health at McGill University
“The fulcrum is the 5S’s — staff, stuff, space, systems, support. That would move the targets up [and our progress against them] where they are meant to be.”
— Carole Mitnick, Global Health and Social Medicine, Harvard Medical School
“Because they’re [children, pregnant women, other ‘vulnerable’ populations] not included in studies of innovations, we become paralyzed. So, when it comes to rolling out innovation, we continue to exclude people with a very perverted notion of protecting them.”
— Jennifer Furin, Global Health and Social Medicine, Harvard Medical School
“We are facing lack of staff … We need integrated teams for TB care, with a MD [medical doctor], nurse, psychologist, nutritionist, and social worker.”
— Rosa Herrera, TB Controller in Baja California, Mexico, and member of the Global TB Community Advisory Board (TB CAB), Americas TB Coalition, and the Mexico TB Social Observatory
“Prevention is still the best key to unlock the door to TB elimination by 2030.”
— Ketholelie Angami, head of the Access to Rights and Knowledge Foundation, Spokesperson of Action TB India, and member of the Global TB Community Advisory Board (TB CAB)
“[referring to short-course prevention and treatment regimens] this is not a dream, these are solutions that exist and, as the TB community, we have a right to demand and access them.”
— Gloriah Kerubo Moses, National Empowerment Network of People living with HIV/AIDS in Kenya (NEPHAK) and member of the Global TB Community Advisory Board (TB CAB)
