After a study suggests that we’ve been using too high a dose of efavirenz for a decade and a half, the move toward scaling up a lower and more cost-effective one faces some hurdles
By Tim Horn and Polly Clayden
Fifteen years after efavirenz was approved by the U.S. Food and Drug Administration (FDA) for the treatment of HIV and went on to become one of the most widely prescribed components of antiretroviral (ARV) therapy worldwide, a question has arisen: have we been using an unnecessarily high dose to treat adults living with HIV?
The question follows the recent publication of clinical trial results demonstrating that 400 mg of efavirenz is no less efficacious—with some evidence of improved tolerability—compared with the standard 600 mg dose, ultimately confirming data from a study completed (but never published) in 1998 suggesting that a lower doses of the drug would suffice. As tempting as it may be to point fingers and rue the possibility of misguided dosing decisions made early in the course of the non-nucleoside reverse transcriptase inhibitor’s development, what’s ultimately important is our ability to capitalize on the better-late-than-never clinical trials results to optimize the drug’s use.
Adapted from: Clayden P. Retrofitting for purpose: treatment optimization. In: Clayden P, Harrington M, Swan T, et al.; i-Base/Treatment Action Group.
2013 pipeline report. New York: Treatment Action Group; 2013.
Efavirenz is sold under the brand names Sustiva and Stocrin and is a component of Atripla and generic single-tablet regimens (STRs). Since its approval in 1998, it has been used in regimens to treat millions of people throughout the world.
Though its efficacy is revered, the side effects of efavirenz are less than ideal—notably, high rates of central nervous system problems that result in approximately 25 percent of people (at least in countries where ARV options are plentiful) discontinuing its use.
The cost of the originator drug has increased steadily (the U.S. wholesale acquisition cost for efavirenz alone is more than $8,500). But the Clinton Health Access Initiative (CHAI)-determined annual ceiling price for generic efavirenz for use in low-income countries is currently US$48 (US$130 for STRs containing efavirenz and tenofovir).
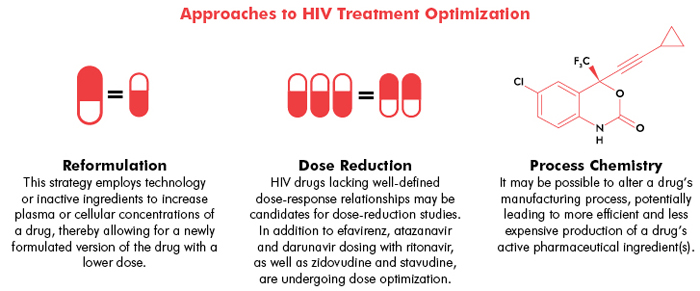
Treatment optimization efforts to improve the tolerability and cost of efavirenz are now under way; these include the study of lower doses that won’t compromise efficacy.
The process by which the 600 mg dose of efavirenz was selected is shrouded in some mystery. According to preliminary data that, curiously, were never published in a peer-reviewed medical journal, a phase II dose-finding comparison (DMP 266-005) of 200, 400, and 600 mg efavirenz suggested comparable viral-load suppression rates after 16 weeks of treatment. In fact, while the clinical trial wasn’t powered sufficiently to determine superiority of one dose over another—each study arm included up to 36 volunteers—81% of those in the 200 mg group, compared with 71% of those taking 600 mg, achieved viral loads below 400 copies/mL, with more than twice the rate of dizziness in the 600 mg group (44% vs. 19% in the 200 mg group).
While FDA approval documents from 1998 note that the 600 mg dose was selected by the manufacturer (then DuPont Merck) to safeguard against the emergence of mutations conferring resistance to efavirenz, it is not clear whether there was sufficient scrutiny of this claim.
More recently, data were reported from two studies involving people living with HIV taking 600 mg of efavirenz and the tuberculosis drug rifapentine. Because of a known interaction between the drugs, rifapentine reduced patients’ blood concentrations of efavirenz to the equivalent of a 400 mg dosing. It did not, however, compromise viral-load suppression rates in either clinical trial.
An official comparison between 400 mg and 600 mg of efavirenz was initiated in 2011, conducted by the Kirby Institute at the University of New South Wales with funding from the Bill & Melinda Gates Foundation. Forty-eight week data from the 96-week ENCORE1 study being conducted at 38 trial sites in 13 countries were initially reported at the 2013 IAS Conference on HIV Pathogenesis, Treatment and Prevention in Kuala Lumpur and published online by the Lancet in February.
Six hundred and thirty individuals were included in the analysis; roughly 68 percent were men, and the distribution of Africans, Asians, and whites was divided evenly into thirds. Median viral load at study entry was 57,000 copies/mL, though roughly 34 percent had viral loads in excess of 100,000 copies/mL. CD4 counts at study entry averaged 273 cells/mm3. Efavirenz was combined with tenofovir/emtricitabine for the study.
At week 48, 94.1% in the 400 mg efavirenz group, compared with 92.2% in the 600 mg group, had viral loads below 200 copies/mL. Lower-dose efavirenz was also found to be “non-inferior” in patients with high baseline viral loads (>100,000 copies/mL), in patients with lower (<22) or higher (>25) body mass indexes, and in ethnic origin comparisons.
Overall, rates of adverse events—including central nervous system–related problems and rash—and treatment discontinuation were similar in the two groups. However, when looking exclusively at adverse events “definitely or probably related to study drugs,” rates of treatment discontinuation were significantly higher in the 600 mg group than the 400 mg group.
Though the tolerability benefits of reduced-dose efavirenz remain uncertain—investigators in the United Kingdom plan to explore this further in a 200 mg dose comparison—the potential for cost savings is tremendous. According to modeling reported by CHAI staff at the Second Conference on Antiretroviral Drug Optimization in April 2012, an efavirenz dose reduction of 33 percent may translate into three-year cost savings of up to US$336 million.
These dollars will be critical to efforts to secure the availability of ART for the 66 percent of the 28.6 million people living with HIV in low- and middle-income countries who are eligible for treatment under the 2013 World Health Organization (WHO) guidelines and lack access to the drugs.
The ENCORE1 study investigators conclude that 400 mg efavirenz should be recommended as part of routine care. However, WHO guidelines are unlikely to reflect this recommendation until additional research is completed, particularly among women in the third trimester of pregnancy (when plasma concentrations of efavirenz are significant reduced) and in areas where TB is endemic and rifampicin-inclusive regimens are routinely prescribed.
Generic manufacturers are prepared to switch to producing STRs containing 400 mg efavirenz, but their incentive to do so hinges on guidance from the WHO and FDA tentative approval in association with PEPFAR.
In the United States and other high-income countries, the results of ENCORE1 may be applicable immediately. But as efavirenz is in the twilight of its patent protection, it is highly unlikely that Bristol-Myers Squibb or Merck (marketers of Sustiva and Stocrin, respectively) will push for the approval of a 400 mg dose. Though 400 mg dosing is possible (two 200 mg capsules), generic drug manufacturers will likely be the first to introduce STRs containing reduced-dose efavirenz and tenofovir—several years from now.•
